Glucose-6-phosphate dehydrogenase deficiency
|
|
| Missing image Merge_articles.png | It has been proposed that this article or section be merged with G6PDH deficiency.
This request may be discussed on the article's talk page. |
Glucose-6-phosphate dehydrogenase (G6PD) deficiency is an X-linked recessive hereditary disease featuring nonimmune hemolytic anemia in response to a number of causes. Its classic association to consumption of broad beans and is commonly known as favism from the Italian name of the broad bean fava.
| Contents |
Signs and symptoms
Patients are almost exclusively male, due to the X-linked pattern of inheritance, but female carriers can have a mild form of G6PD. G6PD manifests itself in a number of ways:
- Prolonged neonatal icterus
- Hemolytic crises in response to:
- Certain drugs (see below)
- Certain foods, most notably broad beans
- Illness (severe infections)
- Very severe crises can cause acute renal failure
Drugs that have been linked to G6PD:
- Primaquine (an antimalarial)
- Sulphonamide antibiotics
- Sulphones (e.g. dapsone, used against leprosy)
- Other sulphur-containing drugs: glibenclamide (an anti-diabetic drug)
- Nitrofurantoin (an antibiotic often used for urinary tract infections)
- Several others[1] (http://www.rialto.com/g6pd/table2.htm)
Diagnosis
The diagnosis is generally suspected when patients from certain ethnic groups (see below) develop anemia, jaundice and symptoms of hemolysis after challenge to any of the above causes, especially when there is a positive family history.
Generally, tests will include:
- Full blood count and reticulocyte count; in active G6PD, "Heinz bodies" (aggregates of protein) can be seen in red blood cells on a blood film;
- Liver enzymes (to exclude other causes of jaundice);
- Haptoglobin (decreased in hemolysis);
- A "direct antiglobulin test" (Coombs' test) - this should be negative, as hemolysis in G6PD is not immune-mediated;
- TSH measurement.
When there are sufficient grounds to suspect G6PD, a direct test for G6PD is the "Beutler fluorescent spot test", which has largely replaced an older test (the Motulsky dye-decolouration test). Other possibilities are direct DNA testing and/or sequencing of the G6PD gene.
The Beutler fluorescent spot test is a rapid and inexpensive test that visually identifies NADPH produced by G6PD under ultraviolet light. When the blood spot does not fluoresce, the test is positive; it can be false-positive in patients who are actively hemolysing. It can therefore only be done several weeks after a hemolytic episode[2] (http://www.uic.edu/pharmacy/services/di/G6PD.htm).
Classification
There are four forms of G6PD:
- Hereditary nonspherocytic hemolytic anemia
- Severe deficiency
- Mild deficiency
- Non-deficient variant
Pathophysiology
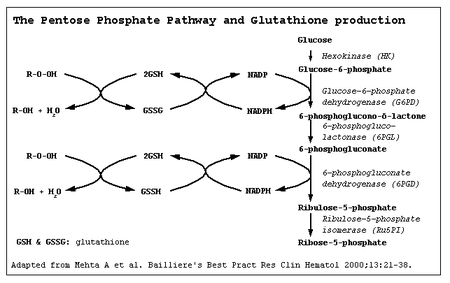
Glucose-6-phosphate dehydrogenase (G6PD) is an enzyme in the pentose phosphate pathway (see image), a metabolic pathway that supplies energy to a number of cells (most notably erythrocytes), and maintains the level of the co-enzyme nicotinamide adenine dinucleotide phosphate (NADPH). The NADPH in turn maintains the level of glutathione in these cells that helps protect the red blood cells against oxidative damage. G6PD converts glucose-6-phosphate into 6-phosphoglucono-δ-lactone and is the rate-limiting enzyme of the pentose phosphate pathway.
Patients with G6PD are at risk of hemolytic anemia in states of oxidative stress. This can be in severe infection, medication and certain foods. Broad beans contain high levels of vicine, divicine, convicine and isouramil — all are oxidants.
In states of oxidative stress, all remaining glutathione is consumed. Enzymes and other proteins (including hemoglobin) are subsequently damaged by the oxidants, leading to electrolyte imbalance, membrane cross-bonding and phagocytosis and splenic sequestration of red blood cells. The hemoglobin is metabolised to bilirubin (causing jaundice at high concentrations) or excreted directly by the kidney (causing acute renal failure in severe cases).
G6PD.png
Although female carriers can have a mild form of G6PD (dependent on the degree of inactivation of the unaffected X chromosome), but homozygous females have been described; in these females there is co-incidence of a rare immune disorder termed chronic granulomatous disease (CGD).
Epidemiology
G6PD is said to be the most common enzyme deficiency disease in the world. A side effect of this disease is that it confers protection against malaria, in particular the form of malaria caused by Plasmodium falciparum, the most deadly form of malaria. A similar relationship exists between malaria and sickle-cell anemia. An explanation is that cells infected with the Plasmodium parasite are cleared more rapidly by the spleen. This phenomenon might have give G6PD carriers an evolutionary advantage.
Treatment
The most important measure is prevention - avoidance of the drugs and foods that cause hemolysis. Vaccination against some common pathogens (e.g. hepatitis A) may prevent infection-induced attacks.
In the acute phase of hemolysis, blood transfusions might be necessary, or even dialysis in acute renal failure. Blood transfusion is an important symptomatic measure, as the transfused red cells are generally not G6PD deficient.
Some patients benefit from removal of the spleen (splenectomy), as this is an important site of red cell destruction. Folic acid should be used in any disorder featuring a high red cell turnover. Although vitamin E and selenium have antioxidant properties, their use does not decrease the severity of G6PD.
References
- Beutler E. G6PD deficiency. Blood 1994;84:3613-36. PMID 7949118.
- Gaskin RS, Estwick D, Peddi R. G6PD deficiency: its role in the high prevalence of hypertension and diabetes mellitus. Ethn Dis 2001;11:749-54. PMID 11763298.
- Mehta A, Mason PJ, Vulliamy TJ. Glucose-6-phosphate dehydrogenase deficiency. Baillieres Best Pract Res Clin Haematol 2000;13:21-38. PMID 10916676.
External links
- Template:OMIM
- Emedicine (http://www.emedicine.com/med/topic900.htm) article on G6PD deficiency
- The G6PD homepage (http://www.rialto.com/g6pd/)