HIV
|
|
| Human immunodeficiency virus | |
|---|---|
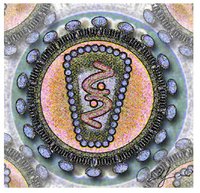 Stylized rendering of a cross-section of the human immunodeficiency virus Template:Taxobox begin placement virus Template:Taxobox group vi entry | |
| Family: | Retroviridae |
| Genus: | Lentivirus |
| Species: | Human immunodeficiency virus 1 |
| Species: | Human immunodeficiency virus 2 |
|}
HIV (Human Immunodeficiency Virus) is a retrovirus that infects cells of the human immune system. It is widely accepted that infection with HIV causes AIDS (Acquired Immunodeficiency Syndrome), a disease characterized by the destruction of the immune system. In the United States and Europe, antibodies to HIV are one of the criteria for a diagnosis of AIDS.
| Contents |
History
HIV has been used since 1986 as the name for the retrovirus that was first proposed as the cause of AIDS by Luc Montagnier of France (who initially named it LAV, Lymphadenopathy-Associated Virus) and by Robert Gallo of the United States (who initially named it HTLV-III, Human T Lymphotropic Virus type III).
UNAIDS estimated that at the end of 2004 there were between 36 and 44 million people around the world living with HIV, of whom 25 million were in sub-Saharan Africa. Global estimates for new HIV infection in 2004 were 4.3-6.4 million. (AIDS epidemic update December 2004 (http://www.unaids.org/wad2004/EPIupdate2004_html_en/epi04_00_en.htm)).
Transmission of HIV
HIV is transmitted through penetrative (anal or vaginal) and oral sex, blood transfusion, the sharing of contaminated needles in health care settings and through drug injection, and between mother and infant during pregnancy, childbirth and breastfeeding according to a leading international health care source UN AIDS in UNAIDS transmission (http://www.unaids.org/en/Resources/faq/faq_transmission.asp#7). The use of physical barriers such as the latex condom is widely advocated to reduce the risk of sexual transmission of HIV.
The WHO estimated in 2000 that 25% of the units of blood transfused in Africa were not tested for HIV and 5% to 10% of cases of HIV infection in Africa were transmitted via blood. [1] (http://www.afro.who.int/press/2001/regionalcommittee/rc51004.html)
Signs and symptoms
The development of antibodies to HIV usually takes place between 6 weeks and 3 months after an infection has occurred. Most people infected with HIV do not know that they have become infected, because no symptoms develop immediately after the initial infection. During the weeks between HIV infection and the development of antibodies to HIV, a person may be highly infectious.
Some people have a glandular fever-like illness (with fever, rash, joint pains and enlarged lymph nodes), in the days following HIV infection (Kahn & Walker 1998).
HIV infection
Hiv-timecourse.png
People who become infected with HIV may have no symptoms for up to 10 years, but they can still transmit the infection to others.
Acute HIV infection progresses over time to asymptomatic HIV infection and then to early symptomatic HIV infection and later, to AIDS, which is identified on the basis of certain infections, grouped by the World Health Organization. Most of these conditions are opportunistic infections that can be easily treated in healthy people.
Most individuals infected with HIV will progress to AIDS if not treated. However, there is a tiny subset of patients who develop AIDS very slowly, or never at all. These patients are called non-progressors.
- Stage I: HIV disease is asymptomatic and not categorized as AIDS
- Stage II: include minor mucocutaneous manifestations and recurrent upper respiratory tract infections
- Stage III: includes unexplained chronic diarrhea for longer than a month, severe bacterial infections and pulmonary tuberculosis or
- Stage IV includes toxoplasmosis of the brain, candidiasis of the esophagus, trachea, bronchi or lungs and Kaposi's sarcoma; these diseases are used as indicators of AIDS.
In 1993, the Centers for Disease Control and Prevention CDC expanded the definition of AIDS to include healthy HIV positive people with a CD4 positive T cell count of less than 200 per mm3 of blood. The majority of new AIDS cases in the United States are reported on the basis of a low T cell count.
WHO recommends that HIV infected adolescents and adults with these infections and/or a T cell count of 200 per mm3 start antiretroviral therapy. (UNAIDS 2005 (http://www.unaids.org/en/Resources/faq/faq_general+information+about+hiv+and+aids.asp#4))
Treatment
HIV infection is a chronic medical condition that can be treated, but not yet cured. There are effective means of preventing complications and delaying, but not preventing, progression to AIDS. At the present time, not all persons infected with HIV have progressed to AIDS, but it is generally believed that the majority will. People with HIV infection need to receive education about the disease and treatment so that they can be active partners in decision making with their health care provider.
A combination of several antiretroviral agents, termed Highly Active Anti-Retroviral Therapy HAART, has been highly effective in reducing the number of HIV particles in the blood stream (as measured by a blood test called the viral load). This can improve T-cell counts. This is not a cure for HIV, and people on HAART with suppressed levels of HIV can still transmit the virus to others through sex or sharing of needles. There is good evidence that if the levels of HIV remain suppressed and the CD4 count remains greater than 200, then life and quality of life can be significantly prolonged and improved.
Treatment guidelines are changing constantly. The current guidelines for antiretroviral therapy [2] (http://www.who.int/docstore/hiv/scaling/summ.html) from the World Health Organization reflect the 2004 changes to the guidleines to defer retroviral treatment in patients with no symptoms who have more than 350 T-cells and viral load under 100,000.
There are several concerns about antiretroviral regimens. The drugs can have serious side effects. Regimens can be complicated, requiring patients to take several pills at various times during the day. If patients miss doses, drug resistance can develop. [3] (http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=12617573&query_hl=1)
In 2004, a possible vaccine was found. In order for the vaccine to work, the patient must first be diagnosed with the virus. Once the patient is treated, T-cell counts have been found to stop dropping. [4] (http://my.webmd.com/content/article/97/104268.htm?z=1727_00000_5024_hv_03)
In 2005, the Centers for Disease Control and Prevention in the United States recommended a 28-day HIV drug regimen for those who believe they may have had contact with the virus. The drugs have demonstrated effectiveness in preventing the virus nearly 100% of the time in those who received treatment within the initial 24 hours of exposure. The effectiveness falls to 52% of the time in those who are treated within 72 hours; those not treated within the first 72 hours are not recommended candidates for the regimen.
Life cycle of HIV
Hiv_gross.png
HIV enters a CD4+ helper T-cell by bonding with either CXCR4 or both CXCR4 and CCR5 depending on what stage the HIV infection is in. A cofactor protein (fusin) is required to assist binding of the viron to the membrane of the T-cell. During the early phases of an HIV infection typically both CCR5 and CXCR4 are bound while late stage infection often involve HIV mutations that only bind to CXCR4.
Once HIV has bound to the CD4+ T-cell a viral protein known as GP41 penetrates the cell membrane and the HIV RNA and various enzymes including but not limited to reverse transcriptase, integrase and protease are injected into the cell.
The host T-cell can process RNA into proteins (as in Polio virus) but this doesn't happen with HIV. Instead, HIV is stabilised by copying it into DNA and inserting it into the host cell's chromosomes. This means the virus can perform more subtle functions by using the host transcription machinery. The virus generates DNA from the HIV RNA using the reverse transcriptase enzyme to perform reverse transcription. This process can be inhibited by drugs. If this succeeds the pro-viral DNA must then be integrated into the host cell DNA using the integrase enzyme. If the pro-viral DNA becomes integrated into the host cell's DNA the cell is now fully infected but not actively producing HIV proteins. This is the latent stage of an HIV infection during which the infected cell can be an "unexploded bomb" for potentially a long time.
To actively produce virus, certain transcription factors need to be present in the cell. The most important is called NF-kB (NF Kappa B) and is present once the T cells becomes activated. This means that those cells most likely to be killed by HIV are in fact those currently fighting infection.
The production of the virus is regulated, like that of many viruses. Initially the integrated provirus is copied to mRNA which is then spliced into smaller chunks. These small chunks produce the regulatory proteins Tat (which encourages new virus production) and Rev. As Rev accumulates it gradually starts to inhibit mRNA splicing. At this stage the structural proteins Gag and Env are produced from the full-length mRNA. Additionally the full-length RNA is actually the virus genome, so it binds to the Gag protein and is packaged into new virus particles.
Interestingly HIV-1 and HIV-2 appear to package their RNA differently - HIV-1 will bind to any appropriate RNA whereas HIV-2 will preferentially bind to the mRNA which was used to create the Gag protein! This may mean that HIV-1 is better able to mutate (HIV-1 causes AIDS faster than HIV-2 and is the majority species of the virus).
The virus starts to form under the cell membrane, in special cholesterol-rich regions, and gradually buds outside. Once outside it has to undergo a maturation step or else it isn't infectious. The virus protease enzyme cleaves Gag into several smaller proteins (Matrix, Capsid, p2, Nucleocapsid, p1 and P6) and this step can be inhibited by drugs. The virus is then able to infect a further cell.
Structure of the virus
HIV looks quite different to the classic retroviruses described in the 1960s. It is around 120nm in diameter (120 billionths of a meter - a red blood cell is around 60 times larger at 7 millionths of a meter) and roughly spherical. There are two forms of the virus. They both consist of a lipid envelope surrounding a protein/RNA core.
Immature form: When the virus leaves the cell it is not infectious and the inner part of the virus particle contains a spherical core (stains dark on electron micrographs). There are also spikes on the outer membrane that are the Env proteins (gp120 and gp41). Sometimes a virus can be seen during the process of budding, when it looks like a dark arc sitting under the cell membrane - this observation meant that HIV was originally classed as a type C retrovirus. The Env proteins link together in groups of three (trimers).
HIV_Viron.png
Mature form: Once the virus protease has cleaved the Gag proteins, the core rearranges into a truncated cone (imagine a traffic cone sliced at an angle across the top!) Some reports also show a small filament linking the core to the membrane. The envelope spikes are often much rarer on mature particles since they are easily dislodged. It is the mature conical core that makes HIV so easily identifiable.
Inside the virus there are two identical strands of RNA, in the same way that we have two identical copies of each chromosome. The RNA is coated by the CA protein (formed from Gag) and is not easily seen unless the virus particles are broken apart. The reverse transcriptase enzyme, which includes integrase, is also packaged into the virus along with certain other important proteins (some from the virus, some captured from the cell) and a tRNA molecule that initiates the reverse transcription process. Because the virus contains certain proteins it needs to replicate, injection of the pure RNA will not result in a successful infection.
HIV has several major genes coding for structural proteins that are found in all retroviruses, and several non-structural or "accessory" genes that are unique to HIV.
General retrovirus genes
- gag. gag-derived proteins make up the cone-shaped viral capsid (p24, i.e. a 24 Kilodalton protein, CA) the nucleocapsid proteins (p6 and p7, NC) and a matrix protein (p17, MA).
- pol. The pol gene codes for the virus enzymatically active proteins. Most important is the so-called reverse transcriptase (RT) which performs the unique reverse transcription of the viral RNA into double-stranded DNA. The latter is integrated into the genome of the host, which means into a chromosome of an infected cell of an HIV-positive person by the pol-encode integrase (IN). Also, pol encodes a specific viral protease (PR). This enzyme cleaves gag- and gag-pol-derived proteins into functional pieces.
- env. env stands for "envelope". The proteins derived from env are a surface (gp120) and a transmembrane protein (gp41). They are located at the outer part of the virus particle and enable the virus to attach to and to fuse with the target cells to initiate the infectious cycle. The gene-product has a knoblike structure.
Specific HIV genes
- tat. A portion of the HIV RNA structure is a hairpin structure which initially prevents full transcription taking place. A small amount of RNA transcripts will be made, however, which allows for the tat protein to be produced. tat binds to CdK9/CycT and phosphorylates it, helping to alter its shape and eliminating the effect of the hairpin RNA structure. This itself increases the rate of trancription, providing a positive feedback cycle. This allows HIV to have an explosive response once a threshold amount of tat is produced, a useful tool in defeating the body's response.
- rev. rev allows fragments of HIV mRNA that contain a rev Response Unit (RRE) to be exported from the nucleus to the cytoplasm. In the absence of rev, RNA splicing machinery in the nucleus quickly splices the RNA so that only the smaller, regulatory proteins can be produced; in the presence of rev, RNA is exported from the nucleus before it can be spliced so that the structural proteins and RNA genome can be produced. Again, this mechanism allows a positive feedback loop and allows HIV to overwhelm the host's defences, and it also provides time-dependant regulation of replication (a common theme in virus infections).
- nef. nef is involved in how pathogenic the virus it. It downregulates the CD4 molecule on T cells (so they can't respond to infections as well). One group of people in Sydney, Australia were infected with a nef-deleted virus and took much longer than expected to progress to AIDS. Unfortunately they did, and a nef-deleted virus vaccine has failed also (in animals - it never made it to human trials).
- vif. vif helps the virus infect cells after it leaves the one it's in. It appears to be involved in how the RNA genome and Gag protein bind to each other and also inhibits a cellular protein that modifies RNA.
- vpr. vpr is involved in getting the virus into the nucleus of the cell so it can integrate. It also causes the cell to stop growing, which can result in immune dysfunction.
- vpu. vpu is involved in getting the virus out of the cell. It enhances virion release from the cell. In HIV-2 the gene is called vpx.
References
- Dybul M, Fauci AS, Bartlett JG, Kaplan JE, Pau AK; Panel on Clinical Practices for Treatment of HIV. Guidelines for using antiretroviral agents among HIV-infected adults and adolescents. Ann Intern Med 2002;137:381-433. PMID 12617573.
- Kahn JO, Walker BD. Acute Human Immunodeficiency Virus type 1 infection. N Engl J Med 1998;331:33-9. PMID 9647878.
See also
- HIV test
- List of HIV-positive people
- HIV positive people
- Criminal Transmission of HIV
- Post Exposure Prophylaxis
External links
- Declaration of Commitment on HIV/AIDS (http://www.un.org/ga/aids/coverage/FinalDeclarationHIVAIDS.html) UN 2001
- Unsafe Health Care and the HIV/AIDS Pandemic (http://www.phrusa.org/campaigns/aids/release080103.html) 2003
- NIH/NIAD/DAIDS (http://www.niaid.nih.gov/daids/)
- HIV/AIDS Treatment Information Service (http://www.hivatis.org)
- Genome (HIV-1) (http://www.ncbi.nlm.nih.gov/entrez/viewer.fcgi?val=NC_001802)
- Genome (HIV-2) (http://www.ncbi.nlm.nih.gov/entrez/viewer.fcgi?val=NC_001722)
- "The Molecules of HIV" information resource (http://www.mcld.co.uk/hiv/)
- AIDS/HIV Education (http://www.ericdigests.org/pre-9212/hiv.htm)
- HIV/AIDS Education in Teacher Preparation Programs (http://www.ericdigests.org/1997-3/hiv.html)
- Continuing medical education about HIV for healthcare providers (http://www.cmeonhiv.com)
- How Aids Works (http://health.howstuffworks.com/aids.htm) (with animation)
- HIV InSite (http://hivinsite.org/InSite)
eo:HIV es:VIH fa:اچ آی وی fr:Virus de l'immunodéficience humaine it:HIV ja:ヒト免疫不全ウイルス nl:HIV no:HIV pl:Wirus nabytego niedoboru odporności pt:HIV ru:ВИЧ simple:HIV sv:HIV zh:人体免疫缺陷病毒
