Tissue engineering
|
|
Tissue engineering can perhaps be best defined as the use of a combination of cells, engineering materials, and suitable biochemical factors to improve or replace biological functions in an effort to effect the advancement of medicine. Probably the first definition of tissue engineering was by Langer and Vacanti who stated it to be "an interdisciplinary field that applies the principles of engineering and life sciences toward the development of biological substitutes that restore, maintain, or improve tissue function”. MacArthur and Oreffo (as cited in "References") defined tissue engineering as "understanding the principles of tissue growth, and applying this to produce functional replacement tissue for clinical use."
In 2003, the NSF published a report titled "The Emergence of Tissue Engineering as a Research Field" (http://www.nsf.gov/pubs/2004/nsf0450/start.htm), which gives a thorough description of the history of this field.
A typical tissue engineering solution consists of a number of parts as alluded to above. This article will discuss each part in turn, along with its implications.
| Contents |
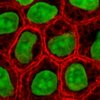
Cells
Tissue engineering solves problems by using living cells as engineering materials. These could be artificial skin that includes living fibroblasts, cartilage repaired with living chondrocytes, or other types of cells used in other ways.
Cells became available as engineering materials when scientists at Geron Corp. discovered how to extend telomeres in 1998. Before this, laboratory cultures of healthy, noncancerous mammalian cells would only divide a fixed number of times, up to the Hayflick limit.
The cells are often categorized by their source. "Autologous" cells come from the same body as that to which they will be reimplanted. "Allogenic" cells come from another body. "Xenogenic" cells come from another species. "Primary" cells are from an organism. "Secondary" cells are from a cell bank.
Autologous cells have the fewest problems with rejection and pathogen transmission—however in genetic disease, suitable autologous cells are not available. In severe burns, autologous cells will not be available in sufficient quantities. Autologous cells also must be cultured from samples before they can be used. This takes time, so autologous solutions are not very quick.
From fluid tissues such as blood, cells are extracted by bulk methods, usually centrifugation or aspheresis.
From solid tissues, extraction is more difficult. Usually the tissue is minced, and then digested with the enzymes trypsin or collagenase to remove the cellular matrix that holds the cells. After that, the cells are free floating, and extracted using centrifugation or aspheresis.
Digestion with trypsin is very dependent on temperature. Higher temperatures digest the matrix faster, but create more damage. Collagenase is less temperature dependent, and damages fewer cells, but takes longer and is a more expensive reagent.
Engineering materials
Cells as found above are generally implanted, or 'seeded' into a scaffold material which serves at least one of the following purposes:
- Enhances structural properties
- Delivers biochemical factors
- Delivers or allows delivery of vital cell nutrients
- Exerts certain mechanical and biological influences to modify the behaviour of the cell phase
Many different materials (natural and synthetic, biodegradable and permanent) have been investigated.
A commonly used material is PLA - poly lactic acid. This is a material which degrades within the human body to form lactic acid, a naturally occurring chemical which is easily removed from the body. This means that during the time that cells are fabricating their own natural matrix structure around themselves, the PLA is able to provide structural integrity within the body, and eventually it will break down, leaving the neotissue (newly formed tissue which will take over the mechanical load).
One of the continuing, persistent problems with tissue engineering is to grow or construct a system of blood vessels to feed an organ. Each layer of cells must be no more than two cell-thicknesses from a source of oxygen. Use of growth factors has been ineffective.
It might be possible to print organs, or possibly entire organisms. A recent innovative method of construction uses an inkjet mechanism to print precise layers of cells in a matrix of thermoreversable gel. Endothelial cells, the cells that line blood vessels, have been printed in a set of stacked rings. WHen incubated, these fused into a tube.
Related topics
- Biomedical engineering is a closely related (and often regarded as parental) field.
External links
- Tissue engineering (http://tissue.medicalengineer.co.uk)
- Pittsburgh Tissue Engineering Initiative (http://www.ptei.org)
- Tissue Engineering Pages (http://wwww.tissue-enginering.net)
Agencies that Support Tissue Engineering Research
References
- Langer, R & Vacanti JP, Tissue Enginering, Science 260(5110), 920-6, 1993 (more than 1000 quotations!)
- MacArthur, B. D. & Oreffo, R. O. C. (6 January 2005). Bridging the gap. In Nature, 433, 19.
- http://www.nsf.gov/pubs/2004/nsf0450/start.htm "The Emergence of Tissue Engineering as a Research Field"
- cell selection for tissue engineering (http://tissue.medicalengineer.co.uk/Sources+of+Cells.php).de:Tissue Engineering