Testosterone
|
|
| 17b-hydroxy-4-androsten-3-one | |
| CAS number [58-22-0] | ATC code G03BA03 |
| Empirical formula | C19H28O2 |
| Molecular weight | 288.43 |
| Bioavailability | ? |
| Metabolism | Liver, Testis and Prostate |
| Elimination half life | 1-12 days |
| Excretion | Urine |
| Pregnancy category | X (USA), Teratogenic effects |
| Physical properties | |
| Melting point | 155–156°C |
| Specific rotation [α]D | +110?2° |
| Standard enthalpy of combustion ΔcH?solid | −11080 kJ/mol |
Testosterone is a steroid hormone from the androgen group. It is the principal male sex hormone and the "original" anabolic steroid.
| Contents |
Sources of testosterone
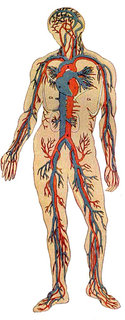
Like other steroid hormones, testosterone is derived from cholesterol. The largest amounts of testosterone are produced by the testes, but it is also synthesized in smaller quantities by the theca cells of the ovaries, the zona reticulosa of the adrenal cortex, and by the placenta. Substantial amounts of the testosterone in women are also produced from estradiol by reverse aromatization in the liver, adipose cells, and other peripheral tissues.
In the testes, testosterone is produced by the Leydig cells. Due to the dual function of the male gonad, testosterone directly influences spermatogenesis. Like most hormones, testosterone is supplied to target tissues in the blood where much of it is transported bound to a specific plasma protein, sex hormone binding globulin (SHBG).
Mechanism of effects
The effects of testosterone in humans and other vertebrates occur by way of two main mechanisms: by activation of the androgen receptor (directly or as DHT), and by conversion to estradiol and activation of certain estrogen receptors.
Free testosterone (T) is transported into the cytoplasm of target tissue cells, where it can bind to the androgen receptor, or can be reduced to 5α-dihydrotestosterone (DHT) by the cytoplasmic enzyme 5α-reductase. DHT binds to the same androgen receptor even more strongly than T, so that its androgenic potency is about 2.5 times that of T. The T-receptor or DHT-receptor complex undergoes a structural change that allows it to move into the nucleus and bind directly to specific nucleotide sequences of the chromosomal DNA. The areas of binding are called hormone response elements (HREs), and influence transcriptional activity of certain genes, producing the androgen effects.Androgen receptors occur in many different vertebrate body system tissues, and both males and females respond similarly to similar levels. Greatly differing amounts of testosterone prenatally, at puberty, and throughout life account for a large share of biological differences between males and females.
The bones and the brain are two important tissues in humans where the primary effect of testosterone is by way of aromatization to estradiol. In the bones, estradiol accelerates maturation of cartilage into bone, leading to closure of the epiphyses and conclusion of growth. In the central nervous system, testosterone is aromatized to estradiol. Estradiol rather than testosterone serves as the most important feedback signal to the hypothalamus (especially affecting LH secretion). In many mammals, prenatal or perinatal "masculinization" the sexually dimorphic areas of the brain by estradiol derived from testosterone programs later male sexual behavior.
Effects of testosterone on humans
In general, androgens promote protein synthesis and growth of those tissues with androgen receptors. Testosterone effects can be classified as virilizing and anabolic effects, although the distinction is somewhat artificial, as many of the effects can be considered both. Virilizing effects include growth of the penis, formation of the scrotum, and deepening of the voice, as well as beard and torso hair. Many of these fall into the category of secondary sex characteristics. When they occur to an unwanted degree in women they are termed "virilization" or "masculinization". Anabolic effects include growth of muscle mass and strength, increased bone density and strength, and stimulation of height growth and bone maturation.
Testosterone effects can also be classified by the age of usual occurrence. For postnatal effects in both males and females, these are mostly dependent on the levels and duration of circulating free testosterone.
Most of the prenatal androgen effects occur between 7 and 12 weeks of gestation.
- Genital virilization (midline fusion, phallic urethra, scrotal thinning and rugation, phallic enlargement)
- Development of prostate and seminal vesicles
Early infancy androgen effects are the least understood. In the first weeks of life for male infants, testosterone levels rise. The levels remain in a pubertal range for a few months, but usually reach the barely detectable levels of childhood by 4-6 months of age. The function of this rise in humans is unknown. It has been speculated that "brain masculinization" is occurring since no significant changes have been identified in other parts of the body.
Early postnatal effects are the first visible effects of rising androgen levels in childhood, and occur in both boys and girls in puberty.
- Adult-type body odor
- Increased oiliness of skin and hair, acne
- Pubarche (appearance of pubic hair)
- Axillary hair
- Growth spurt, accelerated bone maturation
- Fine upper lip and sideburn hair
Advanced postnatal effects begin to occur when androgen has been higher than normal adult female levels for months or years. In males these are normal late pubertal effects, and only occur in women after prolonged periods of excessive levels of free testosterone in the blood.
- Phallic enlargement (including clitoromegaly)
- Increased libido and erection frequency
- Pubic hair extends to thighs and up toward umbilicus
- Facial hair (sideburns, beard, mustache)
- Chest hair, periareolar hair, perianal hair
- Increased muscle strength and mass
- Deepening of voice
- Growth of spermatogenic tissue in testes, male fertility
- Growth of jaw and remodelling of facial bone contours
- Completion of bone maturation and termination of growth (via estradiol metabolites)
"Adult testosterone effects" are important in adult males, and may decline as testosterone levels decline in the later decades of adult life.
- Maintenance of muscle mass and strength
- Maintenance of bone density and strength
- Libido and erection frequency
- Mental and physical energy
Therapeutic use of testosterone
Testosterone was first isolated from a bull in 1935. There have been many pharmaceutical forms over the years. Forms of testosterone for human administration currently available in North America include testosterone cypionate and enanthate in oil for injection, methyltestosterone tablets for oral ingestion, and skin patches and a gel preparation for transdermal absorption. A buccal oral preparation is also available. In the pipeline are a "roll on" delivery method and a nasal spray. Both are under development.
The original and primary therapeutic use of testosterone is for replacement in males who lack it (hypogonadism). When used for this purpose, the benefits of body development, physical strength, and mental energy can be dramatic and side effects rare.
However, over the years, as with every hormone, testosterone or other anabolic steroids has also been given for many other conditions and purposes besides replacement, with variable success but higher rates of side effects or problems. Examples include infertility, lack of libido or erectile dysfunction, osteoporosis, penile enlargement, height growth, bone marrow stimulation and reversal of anemia, and even appetite stimulation. By the late 1940s testosterone was being touted as an anti-aging wonder drug (e.g., see Paul de Kruif's The Male Hormone) in exactly the same way that growth hormone is being described today.
Anabolic steroids have also been taken to enhance muscle development, strength, or endurance. After a series of scandals and publicity in the 1980s (such as Ben Johnson's improved performance at the 1988 Summer Olympics), prohibitions of anabolic steroid use were renewed or strengthened by many sports organizations, and it was made a "controlled substance" by the United States Congress.
The "testosterone deficiency" of aging and the andropause controversy
The latest development in testosterone use appears to be a reprise of the anti-aging claims. A number of physicians, supported by pharmaceutical manufacturers, are popularizing the concept that the testosterone decline of aging (which they term the "andropause") is unnecessary and can be treated. Many endocrinologists suspect that this issue will play out like post-menopausal estrogen replacement: use will increase until large trials demonstrate (1) the benefits are much less dramatic or assured than when treating deficiency, and (2) a higher incidence of side effects will occur associated with this type of use.
Testosterone is often administered to transmen (female-to-male transsexual and transgender people) as part of the hormone replacement therapy.
Synthesis
Testosterone is synthesized from progesterone, the precursor of all steroid hormones and a derivative of cholesterol.
Missing image
Reaction-Progesterone-Androstendione.png
Image:Reaction-Progesterone-Androstendione.png
The synthesis of all androgens starts with the hydroxylation of C-17 of progesterone, to yield 17α-hydroxyprogesterone. The side chain is cleaved to form androstendione.
Missing image
Reaction-Androstendione-Testosterone.png
Image:Reaction-Androstendione-Testosterone.png
The keto group on C-17 is reduced to an alcohol to yield testosterone. Testosterone is the precursor of estradiol.