Atrial flutter
|
|
Atrial flutter is a rhythmic, fast rhythm that occurs in the atria of the heart. This rhythm occurs most often in individuals with organic heart disease (ie: pericarditis, coronary artery disease, and cardiomyopathy).
Atrial flutter is typically not a stable rhythm, and frequently degenerates to atrial fibrillation. However, it may persist for months to years.
| Contents |
|
|
Overview
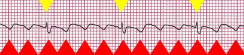
| Atrial flutter with 4:1 block. Flutter waves (red triangles) at rate of 240 / minute. QRS complexes (yellow triangles) at rate of 60 / minute. |
Atrial flutter is a regular, rhythmic tachycardia originating in the atria. The rate in the atria is over 220 beats/minute, and typically about 300 beats/minute. The morphology on the surface EKG is typically a sawtooth pattern.
The ventricles do not beat as fast as the atria in atrial flutter. The AV node acts as a safety valve in the event of any fast rhythm of the heart, including atrial fibrillation and atrial flutter. The AV node slows down conduction of the electrical activity, and if it receives the next action potential before it is ready, the impulse will be blocked at the AV node level, and never reach the ventricles.
In the case of atrial flutter, there is a very particular block pattern at the AV node level. In atrial flutter, the AV node typically will block every other electrical impulse, or three out of four impulses. If every other impulse is blocked, known as 2:1 block, while the atrial rate is 300 beats/minute, the ventricular rate will be 150 beats/minute. If three out of four beats are blocked, known as 4:1 block, while the atrial rate is 300 beats/minute, the ventricular rate will be 75 beats/minute.
In many individuals, the degree of block is variable - sometimes every other beat is transmitted, sometimes two beats are dropped before the third is transmitted, etc. This is known as varying block. For reasons that are not well understood, a stable 3:1 block is not commonly seen in individuals with atrial flutter. A single individual can have varying degrees of block at different times. The varying degree of block is due to a multitude of factors, including catecholamine release and the use of any drugs that inhibit conduction through the AV node, such as beta blockers, digitalis, and calcium channel blockers.
The term 2:1 block comes from the fact that for every two electrical impulses that reach the AV node, only one is transmitted to the ventricle. Similarly, 4:1 block comes from the fact that for every four impulses that reach the AV node, only one is transmitted to the ventricle.
Mechanism of action
Atrial flutter is caused by a reentrant rhythm in either the right or left atrium.
Types of atrial flutter
There are two types of atrial flutter, known as type I and type II.1 Most individuals with atrial flutter will manifest only one of these types of atrial flutter. Rarely someone may manifest both types of flutter; however, they can only manifest one type at a time.
Type I flutter
|
Missing image Common_Flutter.png 12 lead EKG of Type 1 Atrial Flutter |
| Type I atrial flutter, counterclockwise rotation with 4:1 AV nodal block. |
Type I atrial flutter, also known as common atrial flutter or typical atrial flutter, has an atrial rate of 240 to 350 beats/minute. However, this rate may be slowed by antiarrhythmic agents.
Type I flutter can be entrained by rapid atrial pacing. This means that the re-entrant rhythm of the flutter can be broken if a stimulus enters the re-entrant cycle at just the right point, breaking the cycle and thereby terminating the atrial flutter. While this can be performed with a pacemaker, it is performed almost exclusively in the electrophysiology lab by pacing the atrium at a rate just above the rate of the atrial flutter. While entrainment may break atrial flutter and cause the individual to revert to a normal sinus rhythm, the rapid atrial pacing may cause the individual to go into atrial fibrillation.
Type I flutter has two subtypes, known as counterclockwise atrial flutter and clockwise atrial flutter.
Counterclockwise atrial flutter
Couterclockwise atrial flutter (known as cephalad-directed atrial flutter) is more commonly seen than clockwise atrial flutter. The flutter waves in this rhythm are inverted in II, III, and aVF.
Clockwise atrial flutter
Clockwise atrial flutter is less common than counterclockwise atrial flutter. The flutter waves are upright in II, II, and aVF in this rhythm.
Type II flutter
Type II flutter is faster than type I flutter, and usually is 340-430 beats/minute.
Unlike type I flutter, the rhythm of type II flutter cannot be entrained by rapid atrial pacing.
Complications
Clot formation
In atrial flutter, as in atrial fibrillation, there is no effective contraction of the atria. In individuals with structural heart disease, this causes stasis of blood in the atria. The stasis of blood leads to formation of thrombus material (clots) within the heart. In the left side of the heart, thrombus is most likely for form in the left atrial appendage. This is important because, since the left side of the heart supplies blood to the entire body, any thrombus material that dislodges from the left side of the heart can potentially embolize to the brain, causing a stroke. Of course, the thrombus material can also embolize to any other portion of the body.
Sudden death
Sudden death is not directly associated with atrial flutter. However, in individuals with a pre-existing accessory conduction pathway, such as the bundle of Kent in Wolff-Parkinson-White syndrome, the accessory pathway may conduct activity from the atria to the ventricles much faster than the AV node. In this case, the atrial rate of 300 beats/minute will lead to a ventricular rate of 300 beats/minute. The ventricles, unable to sustain a ventricular tachycardia at such a high rate, will go into ventricular fibrillation, which will quickly lead to hemodynamic collapse and death.
Treatment
In general, atrial flutter should be treated the same as atrial fibrillation. Both rhythms do not provide effective contraction of the atria. Because of this, there is stasis of blood in the atria. This stasis of blood leads to the potential formation of thrombus material in the atria. Therefore, individuals with atrial flutter require some form of anticoagulation or anti-platelet agent.
In addition to the treatments available to individuals in atrial fibrillation, there are a couple of treatment considerations that are particular to individuals with atrial flutter.
Ablation
Because of the reentrant nature of atrial flutter, it is possible to ablate the circuit that causes atrial flutter. This is done in the electrophysiology lab by causing a ridge of scar tissue that crosses the path of the circuit that causes atrial flutter.
Rate control
Control of the ventricular rate in atrial flutter may be more difficult than if the individual was in atrial fibrillation. This is because of properties of the AV node. In atrial fibrillation, the AV node is typically bombarded with signals from the atria at rates in excess of 400 beats/minute. This causes a high degree of block within the AV node, with many signals partially penetrating the node and blocking at the lower levels of the AV node. This phenomenon is known as concealed conduction. In atrial flutter, on the other hand, the AV node receives signals very rhythmically at a rate of about 300/minute. Since the atrial flutter is an organized rhythm of the atria, the block at the AV node will be consistently at the same level, and paradoxically a higher number of impulses will get through per minute.
Because of this, it may be easier to control the rate of some individuals if they are converted from atrial flutter to atrial fibrillation. While there are no guidelines for this procedure at this time, this may be attempted in the electrophysiology lab by pacing the atria at rates well over 300 beats/minute.
References
- Chou's Electrocardiography in Clinical Practice, Fifth Edition, Surawicz & Knilans, ISBN 0-7216-8697-4
- Electrophysiologic Testing, Richard N. Fogoros, Blackwell Science, ISBN 0-632-04325-3